|
SEARCH My Blog (Opens in new tab)
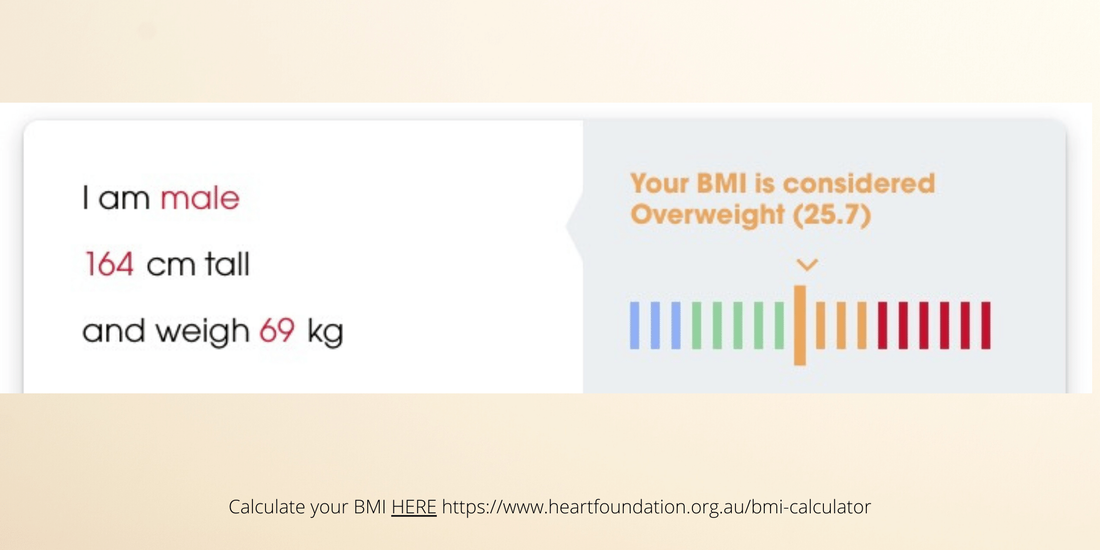
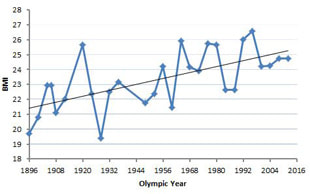
How to stop trending towards “skinny-fat” as you ageCalculating your body mass index (BMI) is one way of trying to work out whether you are within a healthy weight range for your height. However, recent research found that a "healthy" BMI was not associated with the longest life - if you are over 65. That's a surprising finding, despite the well-known limitations of the BMI as a predictor of good health. Let's examine some of those limitations and then review the implications of the research for over 65s. You can calculate your BMI here. BMI has a fundamental flawThe limitations of BMI are manyfold, but they come down to one fundamental "flaw", which is this: BMI is a surrogate measure of body fatness. This means that BMI does not measure body fatness directly but rather, as a proxy measure of body fat. It is directly a measure of excess weight - rather than excess body fat. If the body composition of "excess weight" was consistent and distributed evenly across the population, and that specific composition was associated with consistent health outcomes, then BMI would be a good indicator of those outcomes. But none of those conditions is true. For example, the BMI of 100m Olympic Champions has increased consistently over the last 100 years. Since the BMI is used to indicate body fat, does this mean that their body fat has increased? Clearly not. Modern sprinters no doubt have lower body fat and more muscle than previous generation sprinters. In this case - for this subset of the population - using body weight as a surrogate measure of body fat is highly inaccurate. Nevertheless, BMI is a useful health indicator and the WHO recommends its use as "the most useful population-level measure of overweight and obesity as it is the same for both sexes and for all ages of adults". For adults, WHO defines overweight and obesity as follows:
However, what recent research uncovered is that for an older population those with an "overweight" BMI had a lower "all-cause" mortality than those with a healthy BMI rating. This applied to both men and women. However, those with a BMI rated as "obesity" did not have lower mortality outcomes than those who were rated "healthy". So more weight — more than being “overweight” — was not better. There is an above-average weight-for-height sweet spot which is associated with longer life (for older people). The researchers postulated that lean body mass, i.e. skeletal muscle, is relatively higher in those in the "overweight" BMI category. This kind of makes sense, as you could think about this hypothesis the other way around. For people over 65, who are not exercising, as their BMI falls down through the "healthy" range, their ratio of fat to lean muscle is quickly increasing. Up to 50% loss of muscle by 70Loss of muscle mass (sarcopenia) occurs at about 1% per year after the age of 30 until age 50, and then an accelerated decline (e.g., 12%-15% per decade in strength) after age 50. That's massive. If your BMI is remaining constant - for example in the "healthy" range - then you are adding the equivalent to your muscle loss in fat as you age. Let's do some math and see what that looks like if you don't exercise:
But this does not explain why an older person with an "overweight" BMI has a lower all-cause mortality than another with a "healthy" BMI. The researchers did not determine a reason. (Personally, I think it is because the surrogate use of weight as a measure of body fat fails to account for sarcopenia. Therefore BMI is a poor indicator of mortality outcomes for those over 65 who do not exercise. The BMI needs to be calibrated to typical population rates of muscle loss.) Reaffirms the importance of maintaining muscleWhat the research reconfirmed is that "greater lean tissue mass was associated with improved cardiovascular and overall prognosis". In other words, the more muscle that you maintain and build through exercise the more likely you are to live longer better. Interestingly, they also found that having a low BMI, below "healthy", was linked to poor outcomes, e.g. "an adverse prognosis". Colloquially, this means that being skinny is not as healthy as people perceive (in the sense of being opposite to fat). No doubt that is because the people in that skinny category - as a population group - have a very low ratio of lean muscle mass to fat due to sarcopenia. That is, they are "skinny fat" - and possibly have the worst kind of fat - visceral fat. What this means is that exercise and retaining as much skeletal muscle as possible is one of the simplest ways to improve your prognosis for a longer better life. And if you are exercising, don't worry if your doctor tells you that your BMI is "overweight". Good luck. See My Many Posts On Exercises For Over 50s HERE On This Blog Follow me on Quora for more health and fitness tips.
If you valued this article >> Follow me Leave a comment >> Share it >> Stay healthy If you have any questions email me and I will get back to you. Latest: get your free customised fitness plan designed uniquely for you.
|
ChoicesSince I was diagnosed at 50 with Type 2 diabetes I've been learning how to do bone-building fitness training which lowers my age. You can too. It's your choice. Walter Categories
All
Archives
May 2023
|
 RSS Feed
RSS Feed